THIS YEAR, AROUND 1,000 Australian men will be diagnosed with testicular cancer, and about 30 will die from the disease. That’s not a lot of people, compared to prostate cancer (more than 24,000 diagnoses and 3,500 deaths) or breast cancer (around 21,000 diagnoses and 3,200 deaths), but testicular cancer is the most common cancer in Australian males aged 20-39 years and the incidence is increasing.
If testicular cancer is caught early, before it spreads to other parts of the body, it’s almost certain that it will be cured.
Treatment requires surgery to remove the affected testicle (it is rare for cancer to occur in both testicles). The operation is usually straightforward, uncomplicated and without any long-term effect. In most patients, the remaining testicle produces enough testosterone for normal body function and enough sperm for fertility. People who are concerned about how they might look with only one testicle can choose to have a prosthetic (fake) one.
All in all, the outcome is pretty good for a disease that could otherwise be life-threatening. You just need to find it early.
How to detect testicular cancer
There’s no national population-based cancer screening program for testicular cancer, like there is for cancers of the breast, cervix or bowel, which offer testing to detect cancer before there are any symptoms. Instead, from puberty onwards, males should examine their own testicles regularly enough to become familiar with how they feel, so that if there are any changes they will notice them. If they feel a lump in a testicle, an increase in size, or a change in consistency (softer or harder than usual) they should see their doctor immediately.
How to perform a testicular self-examination
Checking your testicles is simple and takes just a few seconds. Here’s how to get the job done.
- Take a warm shower – warm water helps you and your scrotum relax so it’s easy to feel your testicles
- Gently hold one testicle at a time and roll it between your fingers and thumb, feeling the entire surface – it should feel oval-shaped and firm, and have a smooth surface
- Check for changes to their size or shape, plus things that don’t belong like lumps, pain or swelling
- If you notice something new, book an appointment with your doctor as soon as possible
Why Aussie men are actually good at taking care of themselves
Men are sometimes unfairly maligned for their health behaviours.
Statements like, “men don’t go to the doctor”, that reference average numbers of Medicare-funded GP visits are misleading. The most recent data show an average of 3.3 visits per year for males and 4.1 per year for females, but these averages do not account for differences in the numbers of visits for males and females. More than 1.6 million males saw a GP just once, compared to just over 1.1 million females, whereas only 700,000 males saw a GP more than 12 times, compared to over 1 million females. A more appropriate comparison would be to compare the proportions of males and females who saw a GP if they needed to: 98.9% of males and 99.1% of females. That’s not much of a difference.
Australian research shows that men monitor their health and make decisions to seek help when they believe they need it based on their experience, the perceived severity of their illness and the limitations it places on their lives.
All this bodes well for testicular self-examination and early detection of testicular cancer. Australian males’ problem-solving approach to health concerns and self-monitoring are exactly what’s needed. They just need to know what they need to do.
Past studies of young Australian men (published in 1999 and 2016) suggest that most of them don’t realise they are in the group most at risk of testicular cancer. Most of them didn’t know how to do a testicular exam. We don’t know how this might have changed in the last decade but recent studies overseas (like this one) suggest things are still pretty bad. Deficiencies in health education in secondary school, and a lack of information from healthcare practitioners have been suggested as causes of the problem. Whatever the cause, men deserve better. They need health information and instruction to help them do better what they already do well: look after themselves.
Learn more about testicular self-examinations here.
Associate Professor Tim Moss is the Health Content Manager at Healthy Male — an Australian not-for-profit that provides evidence-based information on men’s health. Tim has a PhD in medicine and uses his experience and expertise from more than 20 years of work in medical research and academia to find and interpret reliable, evidence-based information, to challenge dogma, myths and misinformation.
Related:
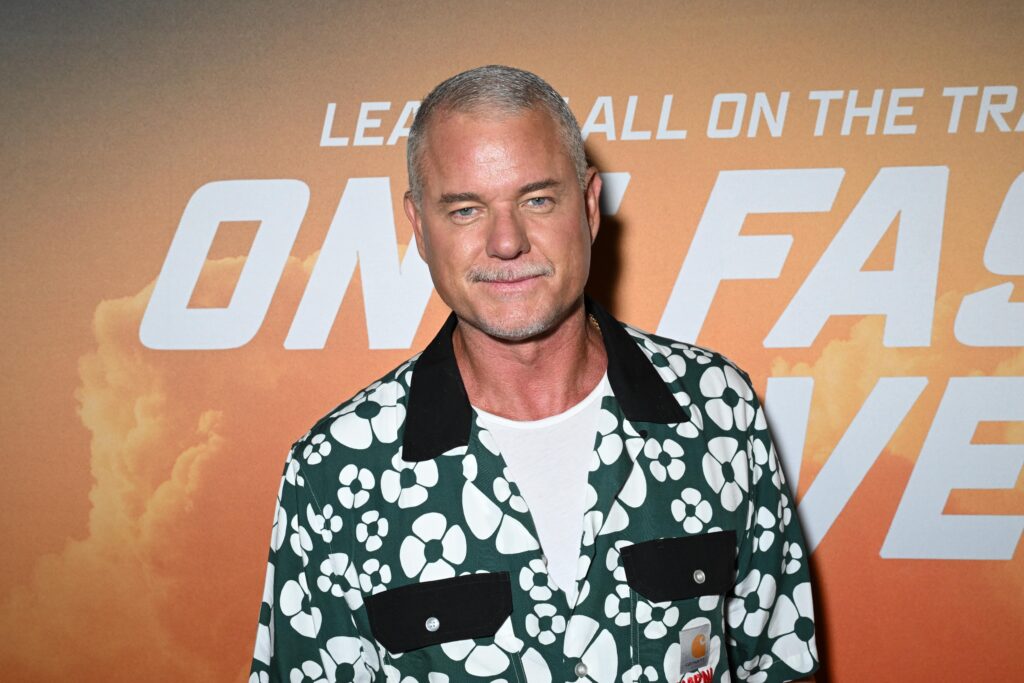
Meet Tom Haddon, a testicular cancer survivor raising awareness and breaking down stigma