By now you know the drill at the doctor’s office: Stick out your tongue. Roll up your sleeve. Drop your drawers. Take a dump in a cup . . . sorry, what?
Okay, maybe you haven’t been asked for a stool sample yet. But a good argument can be made for shipping some of your poo to a lab. Your feaces can reveal a lot about your microbiome – the community of microbial organisms that lives on your skin and inside your nose, your mouth and especially your gut. You have 100 trillion of these creatures, and an unhealthy biome can cause a range of problems from acne to anxiety, says Dr George Weinstock, of the US-based Jackson Laboratory for Genomic Medicine.
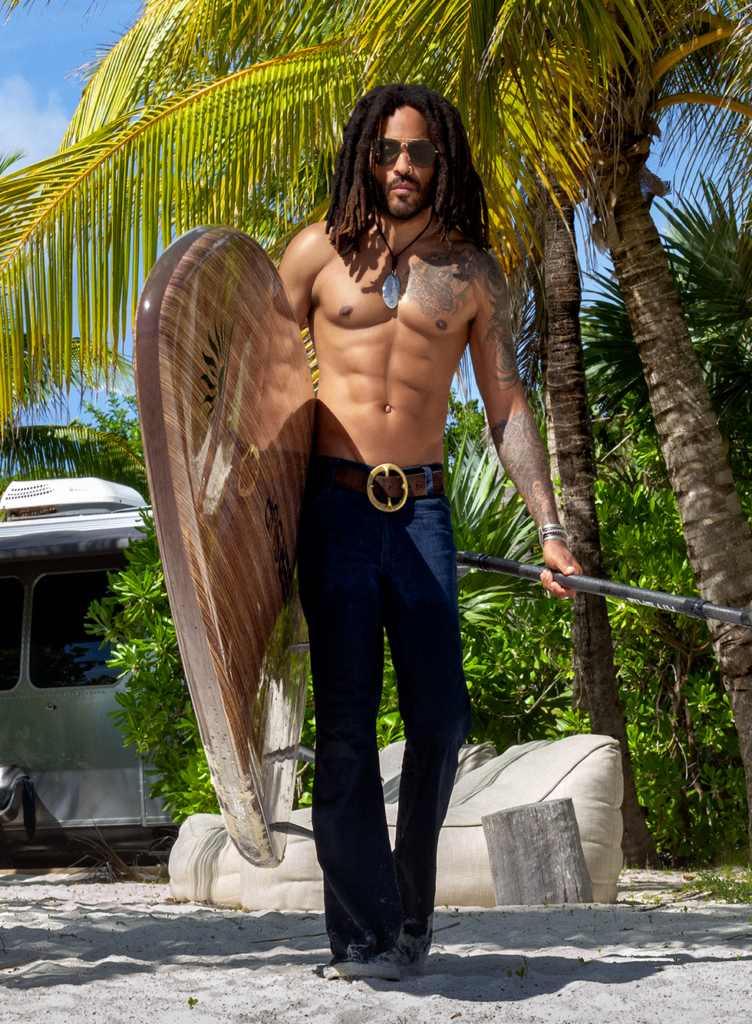
Gut bacteria flourish on fibre. Make sure yours are well fed by eating about 42 grams of fibre daily, the equivalent of three cups of black beans
These microbes are part of you. There are 10 of them for every one of your human cells and together they make up the “superorganism” that is you, says Weinstock. You pilot the ship, but your microbial minions man the turrets. They offer first-line defences against pathogen invasions and signal your immune system when more antibodies are needed for backup.
Diversity is critical: generally speaking, a wider range of microbes creates stronger protection from chronic health conditions and autoimmune diseases. Depression, type 1 diabetes, obesity, even cancer – your risk of developing any of these maladies drops when your microbiome is as lush as a rain forest.
To see how normal men fare, we created a contest: two volunteers swabbed some used toilet paper and sent the samples to a lab to learn whose gut was more diverse.
Volunteer one: Adam Smith, 24.
History of acne and gastrointestinal problems. He controls both by avoiding grains, gluten and sugar.
Volunteer two: Craig Merrick, 40.
Gym owner who eats a healthy, well-rounded diet and works out hard four days a week. His biggest health threat is stress, which can cause inflammation and throw off gut bacteria.
About a month later, the results were in: both guys had above-average biodiversity scores (see “Sign Up for Medical Stool!”). But Smith had less biodiversity than Merrick – predictable, given Smith’s problems. “If not for his diet changes, his microbiome would probably have been much worse,” says Weinstock. And both guys could still probably improve: a 2014 study in Proceedings of the National Academy of Sciences reports that the average microbiome of a Western adult is about a third less diverse than those of our ancestors and people in less developed countries. That may be partly due to our heavily processed diet and the overuse of antibiotics that wipe out good bacteria along with the bad.
Hack your microbiome with these tips and you’ll see an uptick in your immune function and overall health.
1/ Feast on Fibre
Gut bacteria love fibre: researchers at NYU have linked an increased intake of fibre from beans, fruits and vegetables with a greater abundance of both Actinobacteria (which produce natural antibiotics) and Clostridia, a class of microorganisms that’s been linked to decreased risk of colorectal cancer. The average fibre intake in the study was 14 grams a day; you’d be wise to aim for almost three times that, which amounts to just under three cups of black beans.
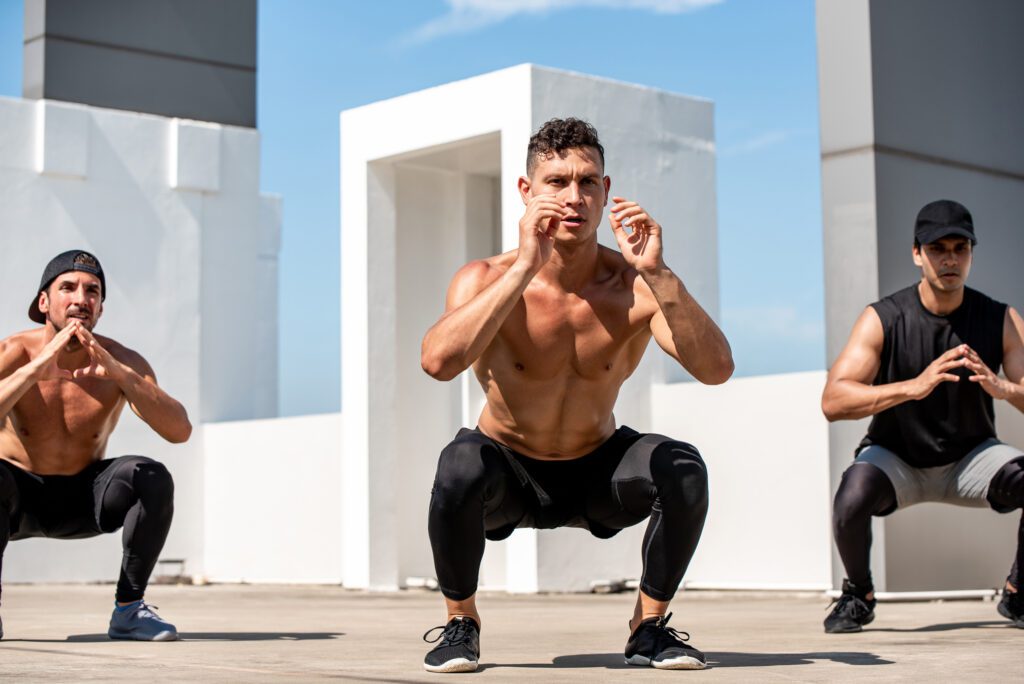
2/ Train Your Gut
You can bolster your biome at the gym. Male pro athletes have significantly more diverse gut bacteria and lower levels of inflammation than less active and sedentary men, a recent study in the journal Gut reports. The researchers aren’t exactly sure how exercise diversifies a person’s microbiome, but the effect may be from a combination of breaking a sweat and eating for performance. The athletes consumed 100 more grams of protein a day than the control group.
3/ Eat Whole Grains
The paleo crowd talks about carbohydrates like they’re poison. Ignore them. In a recent study from the University of Nebraska, healthy adults who consumed 60 grams of wholegrain cereal every day experienced significant improvements in metabolism, immune function and microbial diversity. Yes, fibre certainly played a role in those results, but the study authors suggest that whole grains might confer additional anti-inflammatory benefits.
4/ Go Easy on the Pills
The current generation of prescription antibiotics are broad-spectrum – in other words, they target good and bad microbes indiscriminately. Recent studies indicate that this can disrupt your microbiome within three days and take up to four years to restore the balance. No, you can’t always avoid antibiotics, but you can ask your doctor for the safest option. For example, a study from Amsterdam’s Academic Medical Centre found that amoxicillin has no effect on microbial composition.
5/ Make it a Double Shot
Coffee’s laxative effect may signal that there’s something positive going on in your digestive tract. Scientists at Zurich’s University Hospital found that drinking three cups of coffee a day could bolster your gut’s levels of Bifidobacterium. They speculate that these beneficial microbes help prevent bad bacteria from moving in and taking up residency in your intestinal tract. Credit probably goes to the slew of beneficial compounds that exist naturally in coffee, such as chlorogenic acids.
MH SHOWDOWN: Sign Up for Medical Stool
We asked two MH readers to donate faecal samples for a head-to-head gut test. The results – a snapshot of biome diversity – are in the pie charts. And those big words? They’re phyla of bacteria. Here’s what they do.
Verrucomicrobia
Bacteria in this group spike after you take antibiotics, and they’ve been linked to obesity.
Actinobacteria
These produce about two-thirds of your gut’s natural antibiotics.
Proteobacteria
The Proteobacteria include a wide variety of pathogens (such as E. coli) that have been linked to inflammatory bowel disease.
Bacteroidetes
Another group of beneficial microbes: Bacteroidetes let excess fat slide through the gut undigested.
Firmicutes
They’re common, but having too many is linked to obesity and irritable bowel syndrome.
VERDICT Merrick wins. “Given that he’s eating well and working out” – two ways to promote biodiversity – “it looks like his microbiome is helping him manage his stress,” says Weinstock. Smith’s inflated Firmicutes reading may be causing discomfort.
CRAIG MERRICK, 40
Verrucomicrobia 0.3%
Actinobacteria 2.8%
Proteobacteria 2.9%
Bacteroidetes 39.9%
Firmicutes 54.0%
ADAM SMITH, 24
Verrucomicrobia 1.8%
Actinobacteria 1.9%
Proteobacteria 1.6%
Bacteroidetes 19.0%
Firmicutes 75.5%
*Very small numbers of bacteria not included in results shown.